

Allergy ears , Do you often deal with stubborn ear pain, pressure, or infections that just won’t quit? Allergies might be the hidden culprit. Many people don’t realize how allergic reactions can lead to inflammation, congestion, and fluid buildup in the ears. Left unaddressed, this can trigger chronic problems that disrupt daily life. The connection between allergies and ear health isn’t obvious, but understanding it can make a real difference in finding relief. Let’s uncover how allergies might be affecting your ears and what you can do about it.
Allergies affect millions of people worldwide and can show up in many forms. They’re not just sneezing and itching—understanding their root causes can help you connect the dots between unexpected conditions, like chronic ear problems and recurring health challenges.
Allergens can come from virtually anywhere in your environment. Some of the most common types of allergies include:
Each allergy impacts individuals differently. Some people might feel mild discomfort, while others may experience severe reactions.

Microscopic image of dust mites on fabric
Photo by Cnordic Nordic
The immune system is like your body’s security guard—it works to identify and fight off harmful invaders. With allergies, this defense system becomes trigger-happy. It mistakes harmless substances, like pollen or pet dander, as threats and attacks them.
Here’s what typically happens:
Think of it like a car alarm that goes off every time a leaf falls on the hood. It’s an overreaction that can sometimes be more harmful than the allergen itself. For example, this chronic inflammation can impact areas like the ears, leading to fluid buildup or reduced drainage in the eustachian tubes.
By understanding these mechanisms, it’s easier to see how allergies can ripple outward to affect various systems in the body.
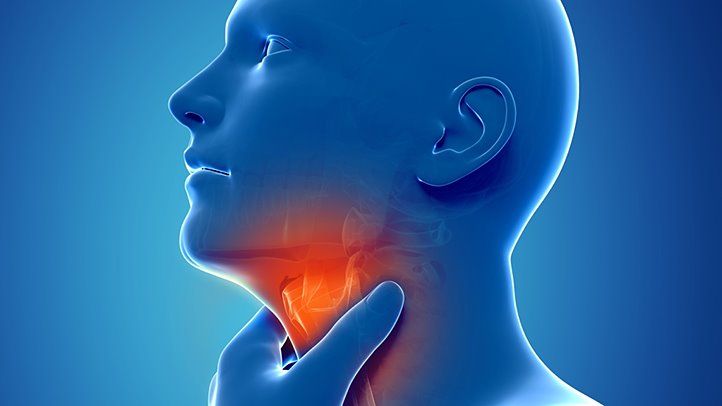
Understanding how the ear functions highlights how allergies can influence ear problems. The ear is not just an organ for hearing—it’s a complex network responsible for both sound and balance. Let’s explore its components and their roles.
The ear is divided into three main sections: the outer ear, the middle ear, and the inner ear. Each plays a unique role in how we hear and maintain equilibrium.
The Eustachian tube, a narrow passage connecting the middle ear to the back of the nasal cavity, acts as the ear’s pressure regulator. Every time you swallow, chew, or yawn, this tube briefly opens. This action equalizes air pressure between the middle ear and the surrounding atmosphere.
Its other functions include:
When the Eustachian tube becomes congested—or blocked due to allergies—imbalances and infections are more likely. Allergies often cause inflammation in this small tube, leading to fluid buildup and pressure, which can spiral into chronic allergy ears issues.
A woman studies anatomy diagrams on a tablet indoors, focusing on educational material.
Photo by RF._.studio
This interconnected structure shows how even minor changes in one part of the ear or the surrounding areas can have cascading effects, especially when triggered by allergies.
Allergy ears don’t just make you sneeze or cause itchy eyes—they can play a major role in persistent ear issues. Many don’t realize that the inflammation and congestion caused by allergic reactions can create a cascade of problems in ear function. Let’s break down the mechanics of how allergies contribute to chronic ear problems.
One of the most common ways allergies wreak havoc on ear health is through fluid accumulation. When allergens like pollen or pet dander activate your body’s defense system, it leads to inflammation and excessive mucus production. This can clog nasal passages and block the drainage pathways of the ears.
This is why individuals with seasonal allergies might notice recurring earaches or infections during high-pollen months.

A woman lying in bed sneezing, illustrating symptoms of allergies affecting overall health.
Photo by Andrea Piacquadio
The Eustachian tube, a small but crucial pathway connecting the middle ear to the back of your throat, manages air pressure and fluid drainage. Allergies are notorious for causing these tubes to malfunction.
Think of the Eustachian tube as the air vent in your car. If that vent is blocked, no airflow gets through, leading to stuffy and uncomfortable conditions.
Sinus congestion doesn’t just make your head feel heavy—it directly impacts your ears too. Allergies can cause swelling in the sinus cavities, which increases pressure around the ear canals.
Understanding the connection between sinus health and ear health highlights just how intertwined these systems are. Managing sinus pressure through allergy treatments can be a crucial step in alleviating chronic ear conditions.
By addressing allergies early, you can reduce inflammation and prevent these complications from becoming long-term issues.
Allergies don’t just affect your nose and throat; they can significantly impact your ears, often leading to long-term discomfort or health issues. If you’re wondering whether that nagging ear trouble could be linked to allergies, you’re not alone. Allergies can cause blockages, swelling, and fluid buildup in the delicate ear structures, resulting in various symptoms. Let’s explore the key signs and symptoms.
Allergic reactions can trigger hearing loss, which may be temporary or, in rare cases, permanent. How does this happen? When allergies inflame the Eustachian tubes, they can’t regulate pressure or drain fluid properly. This fluid buildup can muffle sounds, creating what’s known as conductive hearing loss.
Think of it this way: If your ears are clogged, it’s like trying to hear through a pair of thick earmuffs. Sounds become muted, and clarity suffers.
Ear pain linked to allergies is often described as a feeling of pressure, fullness, or throbbing discomfort. Allergies can cause swelling in the middle ear or around the Eustachian tubes, disrupting normal function.
Signs of ear pain caused by allergies include:
Allergy-induced discomfort is similar to how you might feel when swimming underwater—pressure builds, and relief feels impossible without proper drainage.
Chronic ear infections are another red flag for allergy-related ear issues. When your body reacts to allergens, it produces excessive mucus and triggers inflammation, creating prime conditions for infections.
The cycle often begins when fluid trapped behind the eardrum becomes a breeding ground for bacteria or viruses. If allergies are left untreated, this cycle can repeat over and over again.

A young child sits on a couch indoors, using a tissue, suggesting illness or allergy.
Photo by cottonbro studio
By addressing the root cause—your allergies—you can often stop these symptoms in their tracks. Don’t let these ear problems linger; whether it’s mild pain or recurrent infections, prompt care can help protect your ear health over time.
Getting to the root of chronic ear issues often starts with identifying whether allergies are to blame. Once diagnosed, treatment can help manage symptoms and prevent further complications. Let’s explore the key steps and options available.
Accurate diagnosis begins with allergy testing, which identifies substances causing your body to overreact. Here are the most common methods used by specialists:
Allergy testing is quick and minimally invasive, providing valuable insights into what’s triggering your symptoms.

A medical professional takes a blood sample from a patient for testing.
Photo by Amornthep Srina
Once allergies are diagnosed, targeted treatment can significantly reduce symptoms and alleviate chronic ear problems. Here are some frontline options:
Combining medications with lifestyle changes, like using an air purifier or avoiding known triggers, offers the best results for allergy management.
Not sure if it’s time to seek professional help? Persistent symptoms could mean it’s time to visit an ENT specialist, especially when:
An ENT (ear, nose, and throat) specialist can assess the complexity of your symptoms and offer advanced treatments like drainage procedures or sinus surgeries to improve ear health.
Recognizing when to seek expert advice is key to stopping chronic ear problems from worsening. Don’t ignore symptoms that impact your daily life—timely action can make all the difference.
Preventing allergies from escalating into chronic ear issues is about proactive care and mindful habits. Allergies and ear health are intricately linked, and taking specific steps can reduce the risk of complications. Let’s dig into what you can do to keep your ears healthy and allergy symptoms at bay.
Avoiding allergens is the first line of defense. While you can’t entirely eliminate allergens, you can minimize exposure with simple lifestyle tweaks:
By reducing overall allergen exposure, you’re giving your immune system fewer reasons to overreact, which can help protect your ears.
 Photo by Gustavo Fring
Photo by Gustavo Fring
Proper ear care is essential to prevent potential ear problems that stem from allergies or infections. Maintaining ear hygiene isn’t about cleaning excessively but doing it safely and effectively.
Taking these steps ensures not only that your ears remain clean but also that you avoid introducing new irritants or infections.
Allergies can quietly lead to chronic ear problems if left untreated. The inflammation, fluid buildup, and pressure they cause can seriously affect ear function over time.
Understanding this connection empowers you to address symptoms early and avoid lasting complications. Simple steps like managing allergens, seeking treatment for allergy symptoms, and consulting a medical professional can protect your ear health.
If allergies are causing discomfort, don’t wait. Tackle the root cause and reclaim control over your quality of life. Have you noticed a link between your allergies and ear issues? Let us know in the comments!





