We recently sat down with a patient who was suffering from TMJ disorder. Dr. Friedman explained to the patient that this disorder was causing pain in his jaw and contributing to his frequent, inconsolable headaches. Then Dr. Goldberg outlined a number of treatment options, including one that came as a bit of a surprise.
“Have you considered Botox therapy for your TMJ?”
Our patient did a double-take, “Botox for TMJ? I’ve never heard of that before, how does that work?”
Here’s what he told him.
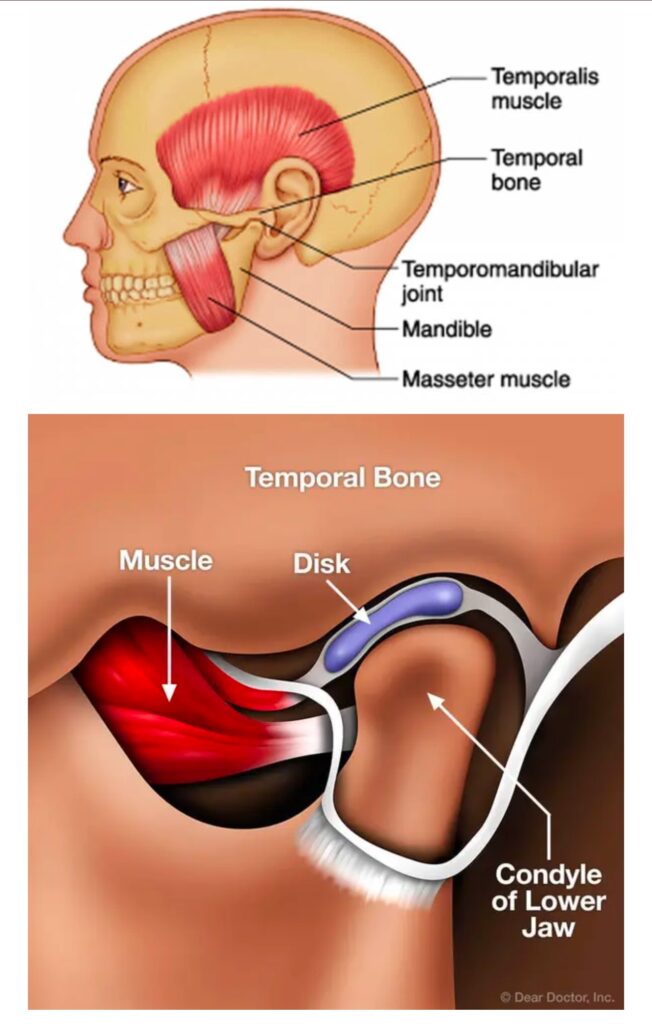
Most people know it as a beauty-enhancing product that gets rid of wrinkles and fine lines in the face. That’s true, it is! But think about what Botox does — it temporarily prevents nerve cell signals from reaching your muscles and reduces abnormal muscle contractions. With this in mind, you can understand how it can be useful for relaxing the muscles around your jaw, too.
In fact, Botox has a long history of medically therapeutic uses, all involving muscular conditions. Currently, Botox is used to treat over 20 different medical conditions, and there are more than 6 million Botox treatments administered each year.
Botox injections have been administered in dentists’ offices throughout the US for many years now. Some dentists do offer Botox as the finishing touch to a cosmetic dental treatment.
Here in our office, the use of Botox in dentistry stems from one important goal… relieving TMJ pain and helping you feel your very best.
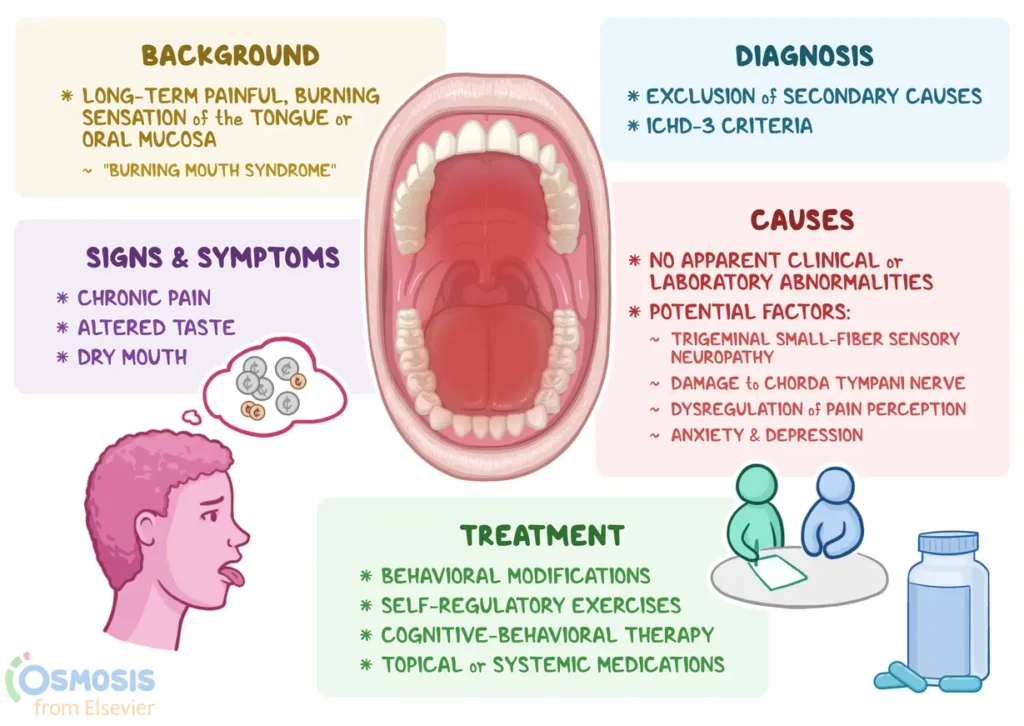
Burning Mouth Syndrome is a chronic condition characterized by a burning or scalding sensation in the mouth, often without any obvious cause. The discomfort can affect the tongue, lips, gums, palate, throat, or the entire mouth. For some, the sensation is mild and intermittent, while for others, it can be severe and persistent, significantly impacting their quality of life.
BMS is more common in middle-aged or older adults, particularly women going through menopause, though it can affect anyone. Despite its prevalence, diagnosing BMS can be challenging because it often overlaps with other oral health issues or systemic conditions.
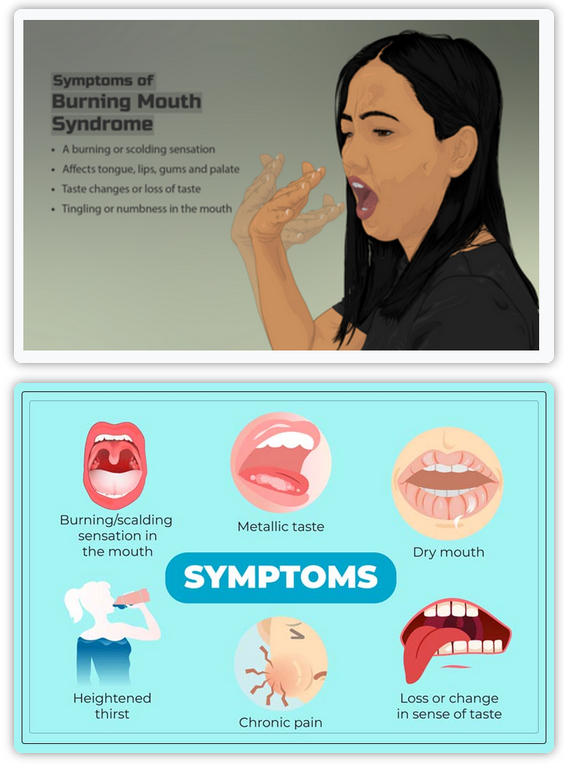
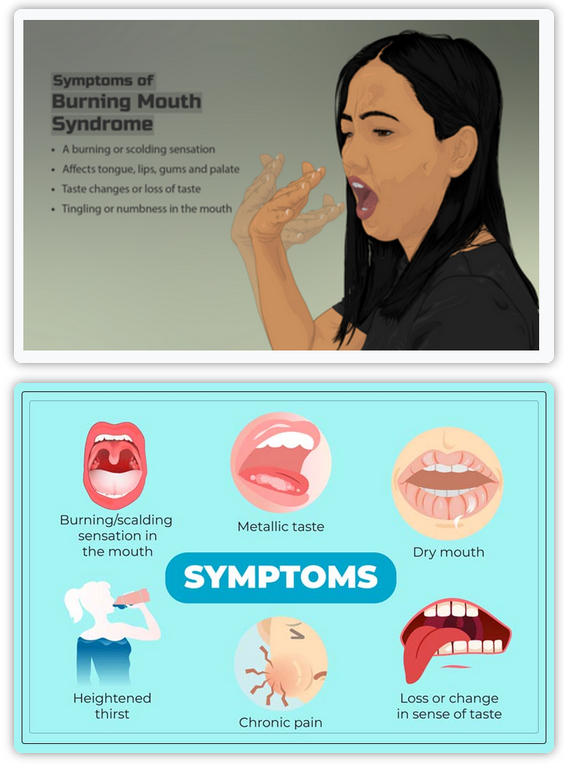
Symptoms of Burning Mouth Syndrome
The primary symptom of BMS is, of course, a burning sensation in the mouth. However, this condition can also present with other accompanying symptoms, such as:
- A dry or sore mouth
- A metallic or bitter taste
- Tingling or numbness in the mouth
- Increased thirst
- Loss of taste or altered taste perception
- Difficulty eating or speaking due to discomfort
The burning sensation may fluctuate throughout the day, often worsening as the day progresses. Some people report temporary relief while eating or drinking, which can make the condition even more perplexing.
The exact cause of BMS is not fully understood, which is why it’s often referred to as a “syndrome” rather than a disease. However, researchers have identified several potential contributing factors, which can be categorized into primary and secondary causes:
1. Primary Burning Mouth Syndrome
When no underlying medical or dental cause can be identified, the condition is classified as primary BMS. It is believed to be related to nerve dysfunction or damage in the oral cavity, possibly involving the nerves responsible for taste and pain.
2. Secondary Burning Mouth Syndrome
Secondary BMS occurs when the burning sensation is linked to an underlying condition or factor, such as:
- Hormonal changes: Menopause is a common trigger for BMS, likely due to fluctuations in estrogen levels.
- Nutritional deficiencies: Deficiencies in vitamins like B12, iron, zinc, or folate can contribute to oral discomfort.
- Oral habits: Teeth grinding, tongue thrusting, or excessive use of mouthwash can irritate the mouth.
- Dry mouth (xerostomia): Reduced saliva production, often caused by medications or medical conditions, can lead to a burning sensation.
- Allergies or irritants: Reactions to dental materials, foods, or oral care products may trigger symptoms.
- Psychological factors: Stress, anxiety, and depression are closely linked to BMS, though it’s unclear whether they cause the condition or result from it.
- Systemic conditions: Diabetes, thyroid disorders, and gastrointestinal issues like acid reflux have been associated with BMS.
Diagnosing Burning Mouth Syndrome
Diagnosing BMS can be a process of elimination. Your healthcare provider or dentist will likely start by reviewing your medical history, conducting a physical examination, and ruling out other potential causes of your symptoms. They may also order blood tests to check for nutritional deficiencies, hormonal imbalances, or other systemic issues.
In some cases, a referral to a specialist, such as an oral pathologist or neurologist, may be necessary to confirm the diagnosis.
While there is no one-size-fits-all cure for BMS, several treatment options can help manage the symptoms and improve your quality of life. The approach will depend on whether your BMS is primary or secondary:
1. For Secondary BMS
If an underlying cause is identified, treating that condition often alleviates the burning sensation. For example:
Addressing nutritional deficiencies with supplements.
Adjusting medications that cause dry mouth.
Managing acid reflux or hormonal imbalances.
2. For Primary BMS
When no specific cause is found, treatment focuses on symptom management. Options may include:
Medications: Low-dose antidepressants, anticonvulsants, or nerve pain medications can help regulate nerve activity.
Topical treatments: Mouth rinses or gels containing lidocaine or capsaicin may provide temporary relief.
Behavioral therapy: Cognitive-behavioral therapy (CBT) can help manage stress, anxiety, or depression associated with BMS.
Lifestyle changes: Avoiding irritants like alcohol, tobacco, and spicy foods, as well as staying hydrated, can reduce symptoms.