- Review on HealthGrade
Torn Earlobe Repair
Visit Website
Location
723 Fitzwatertown Road Willow Grove, PA 19090
See Dr. Goldberg’s profile on Healthgrades.
Call Us
(215) 659-8805
URGENT CARE ENT
Same day appointments
(215) 659-8805
Visit Website
723 Fitzwatertown Road Willow Grove, PA 19090
(215) 659-8805
Same day appointments
(215) 659-8805
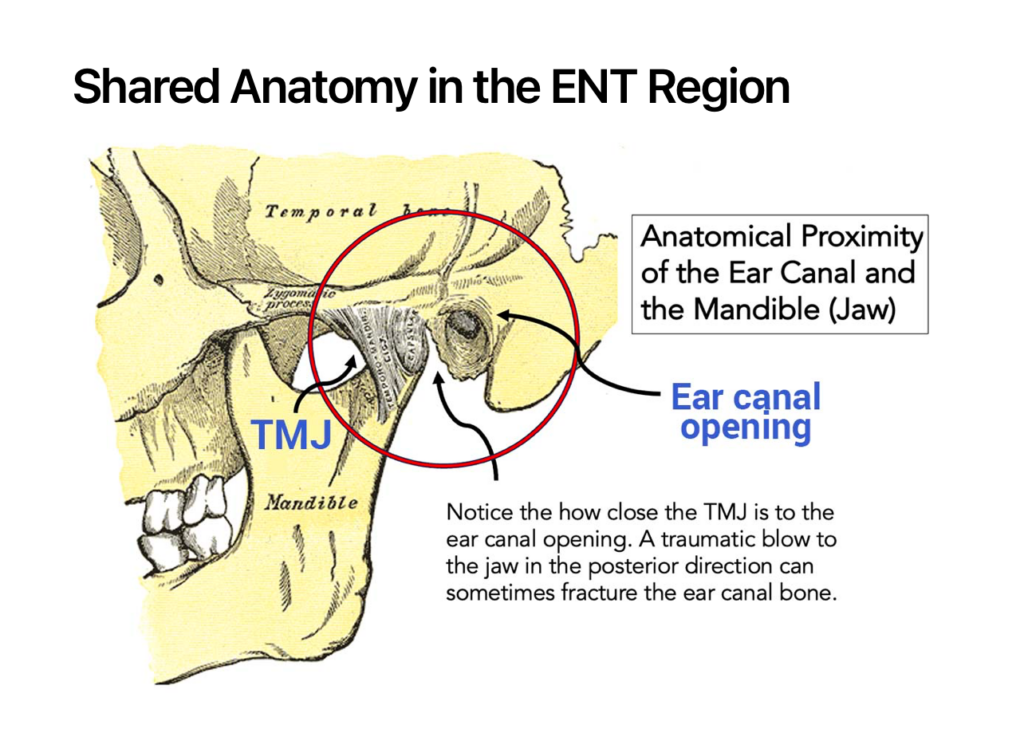
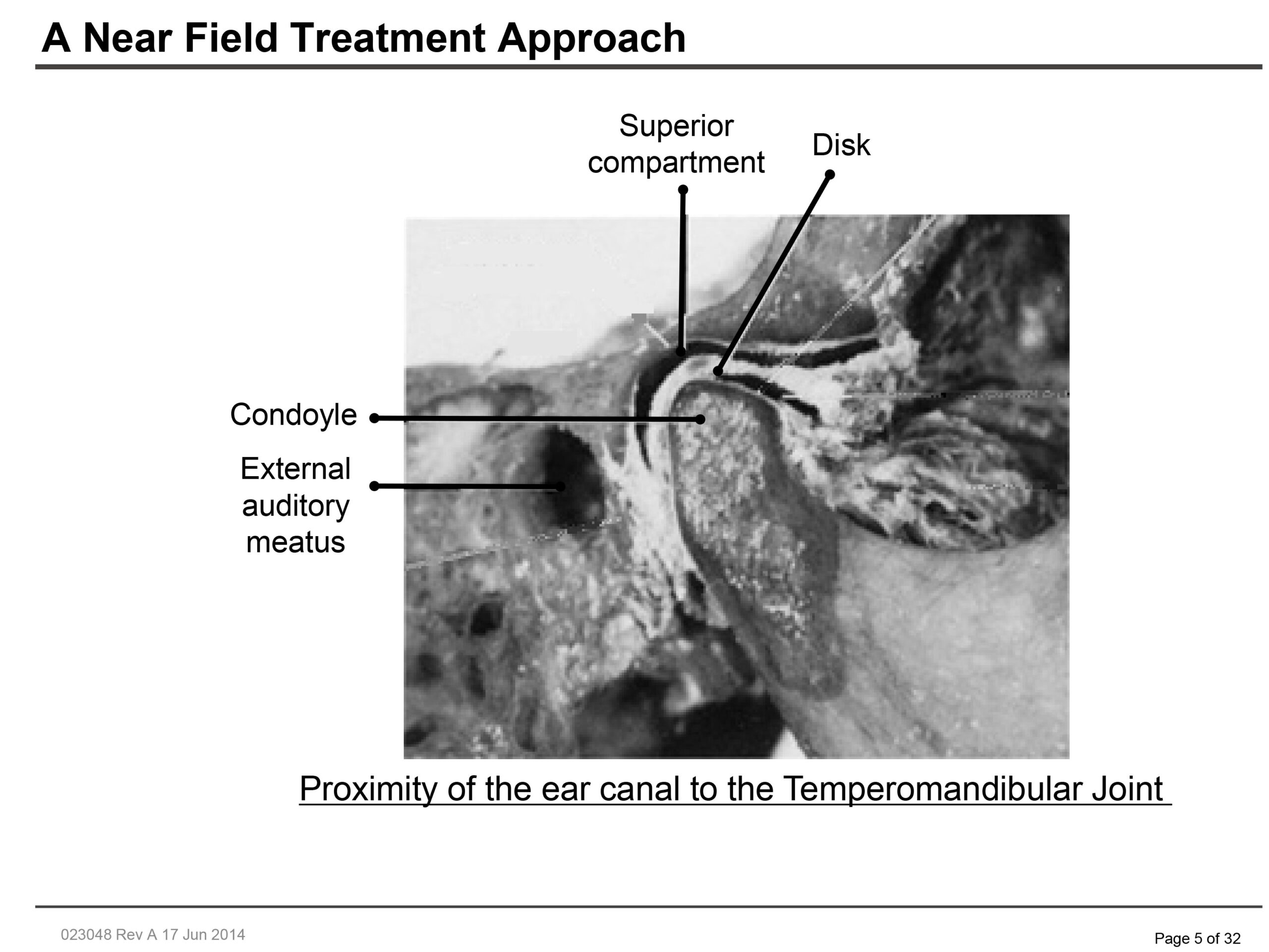
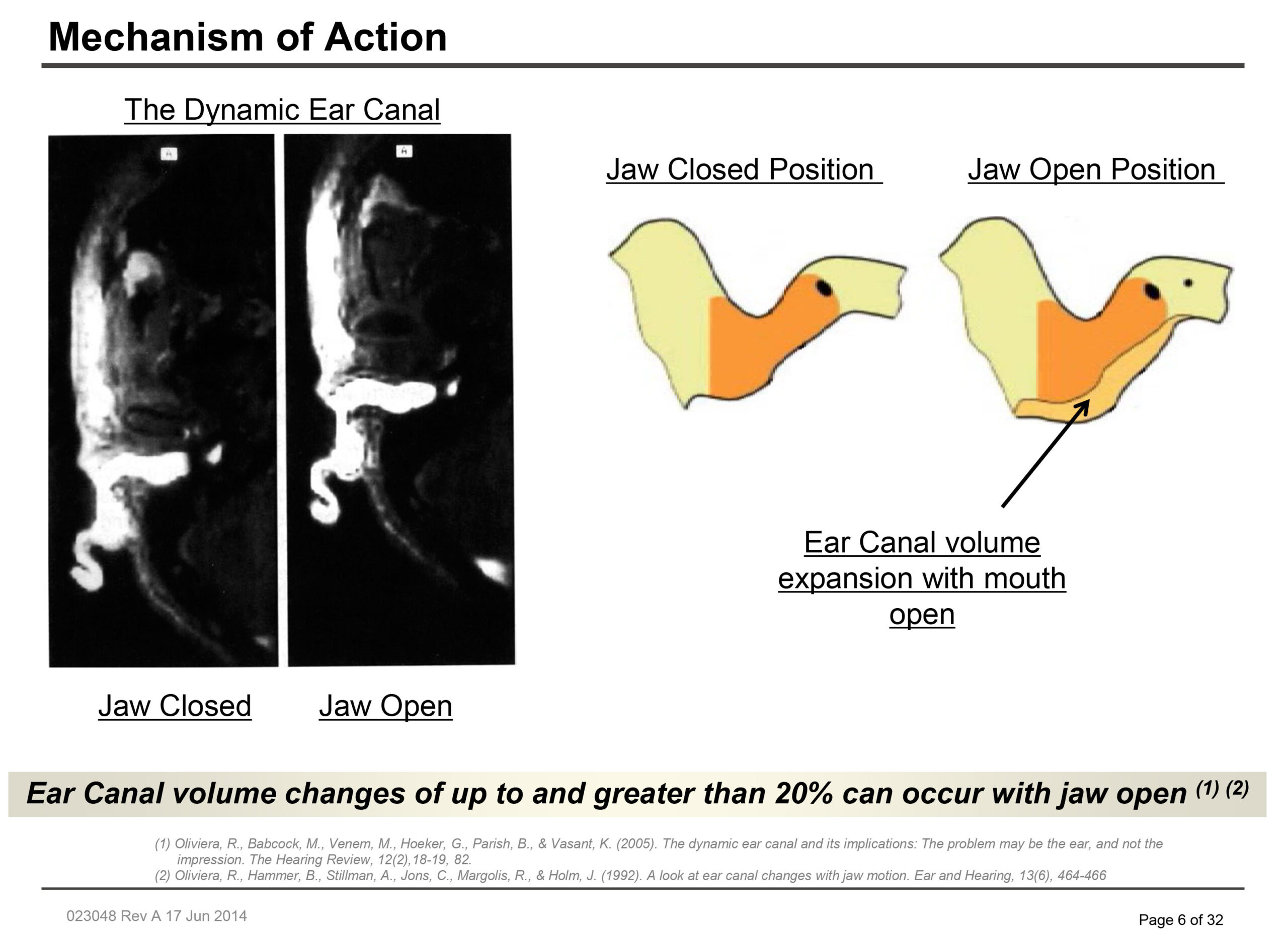
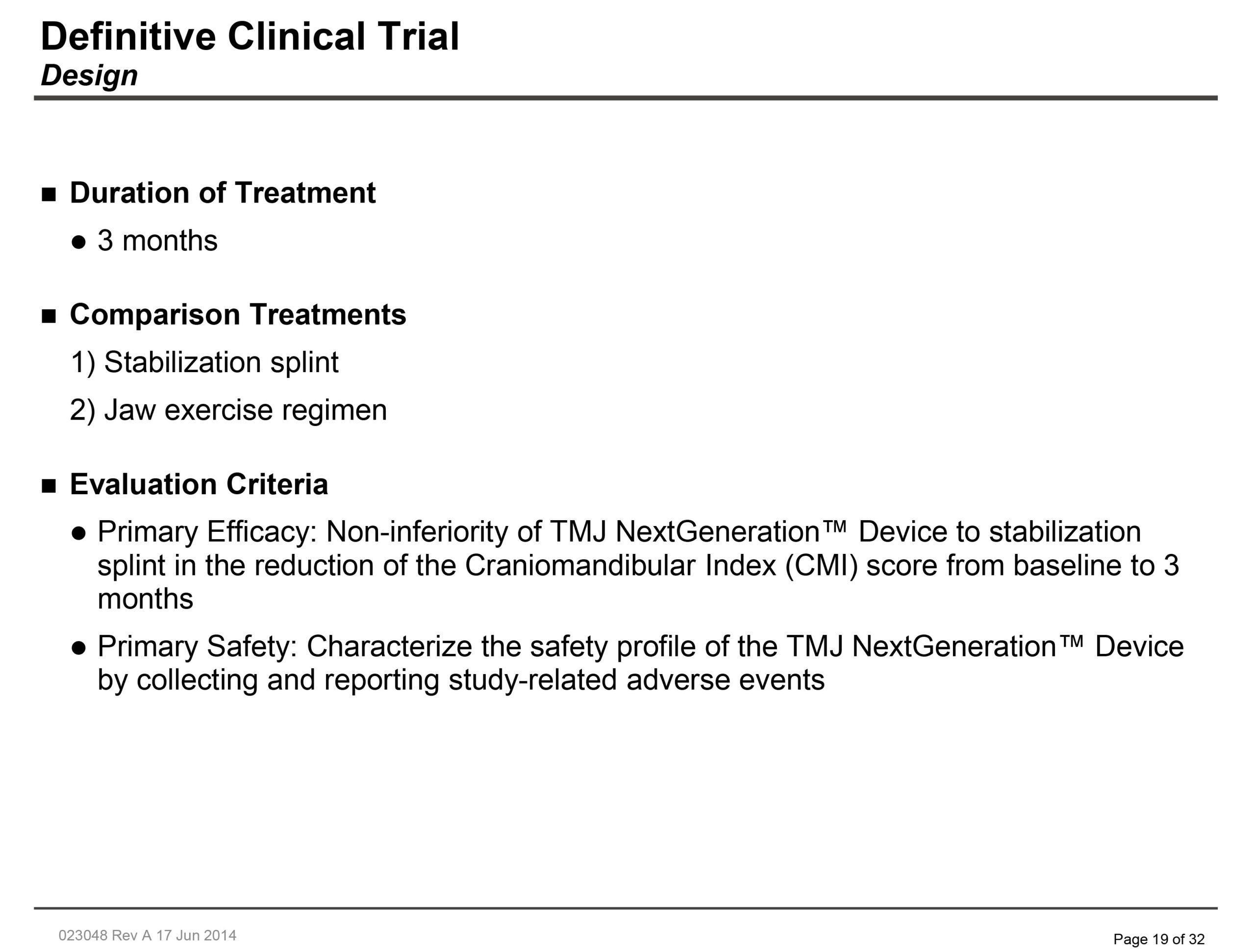
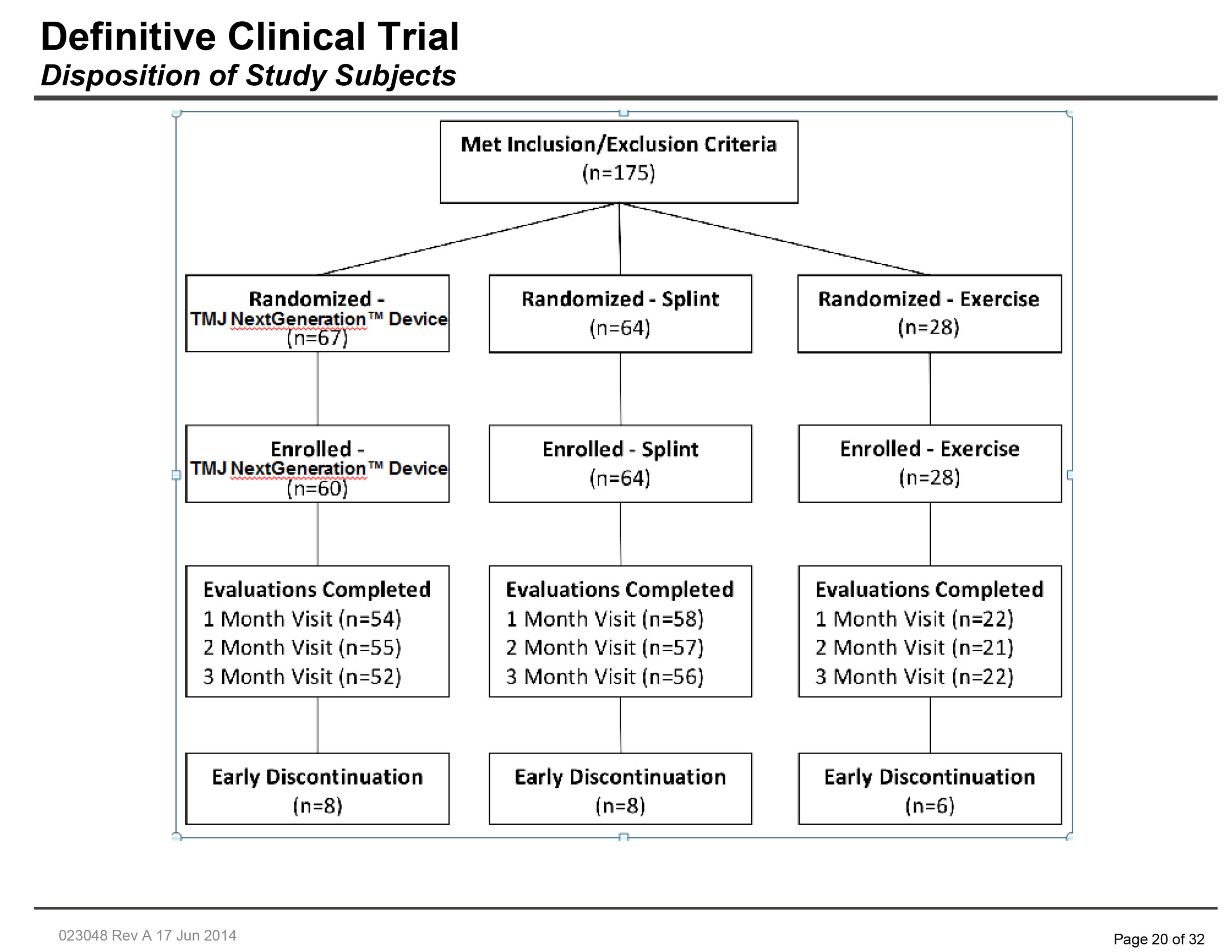
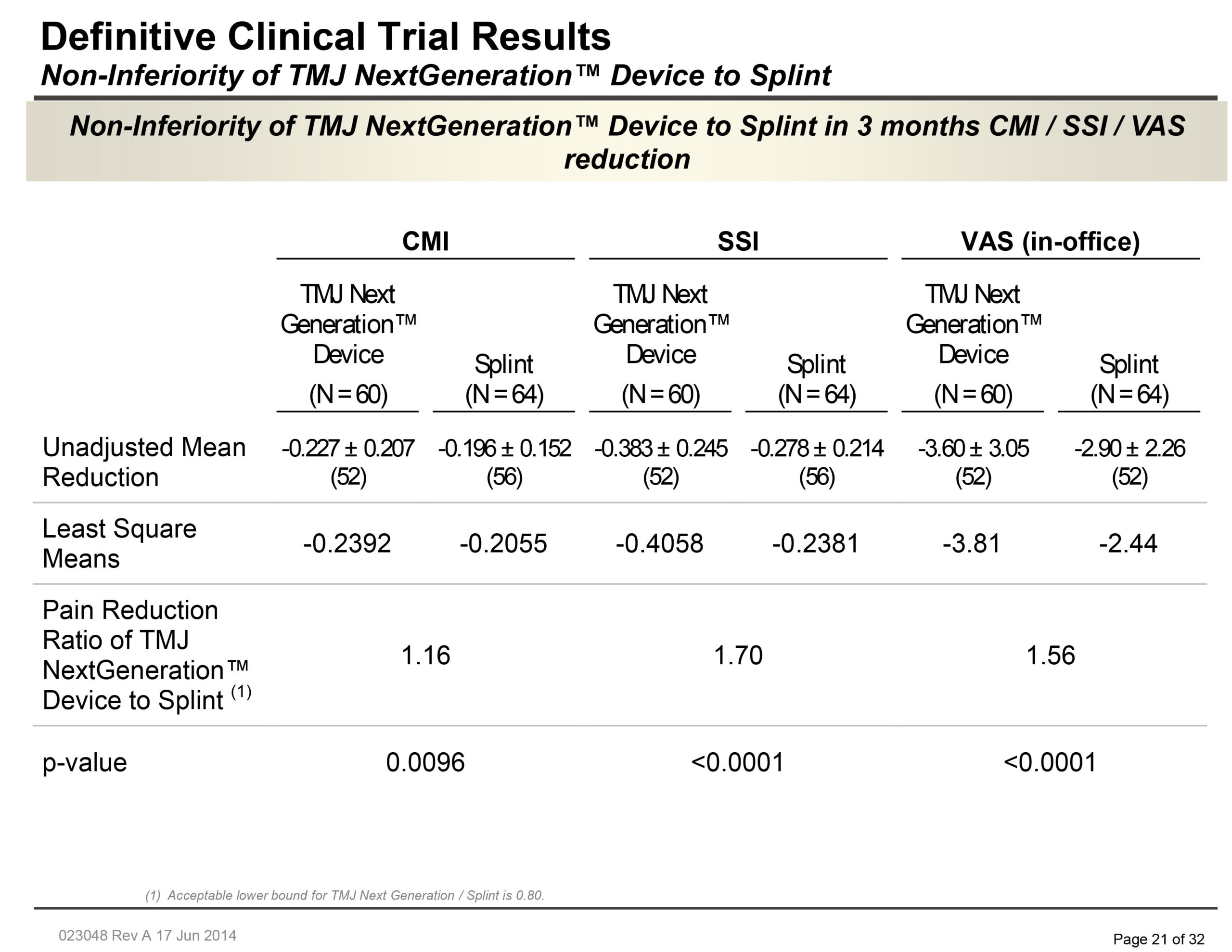
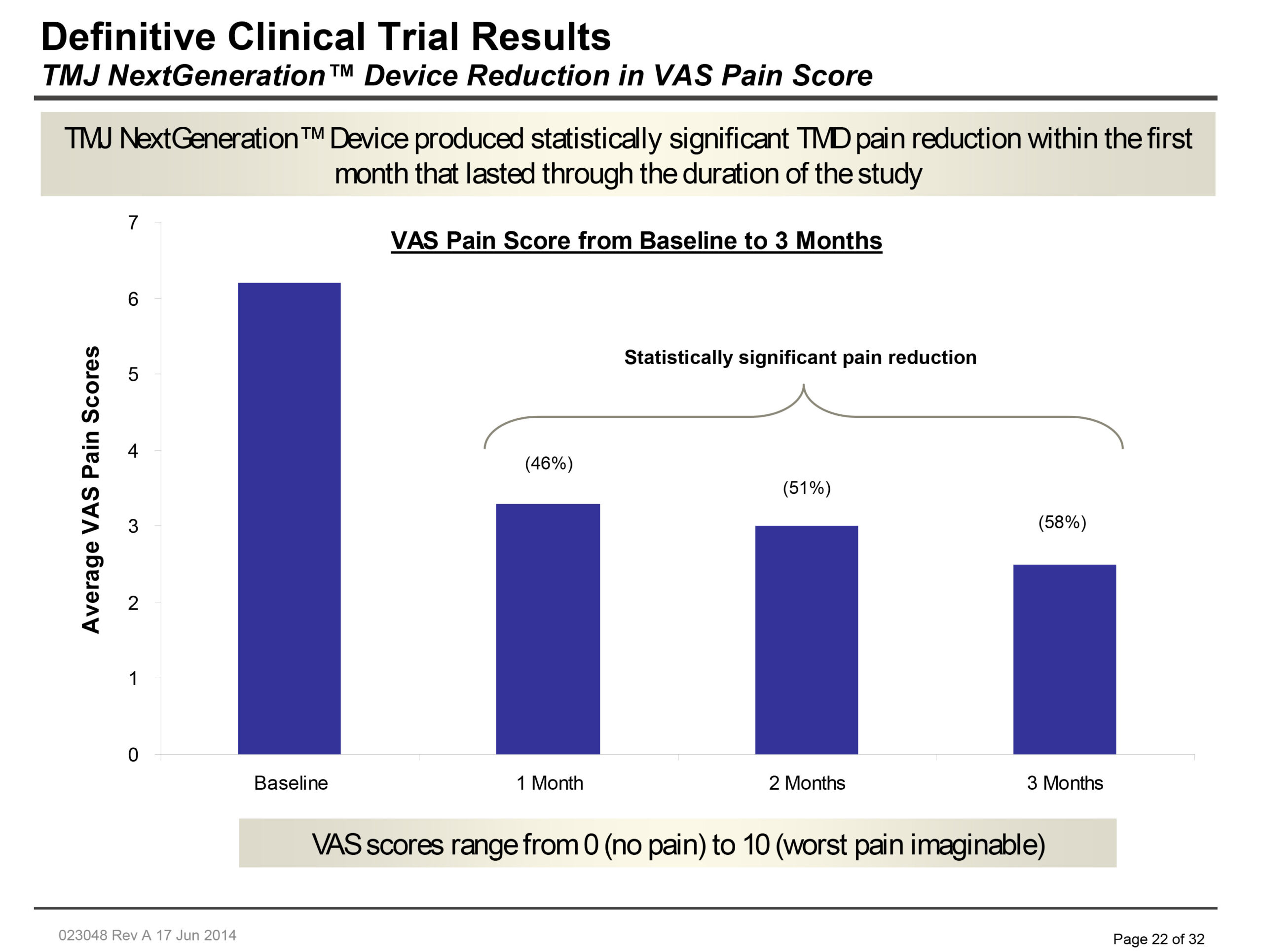
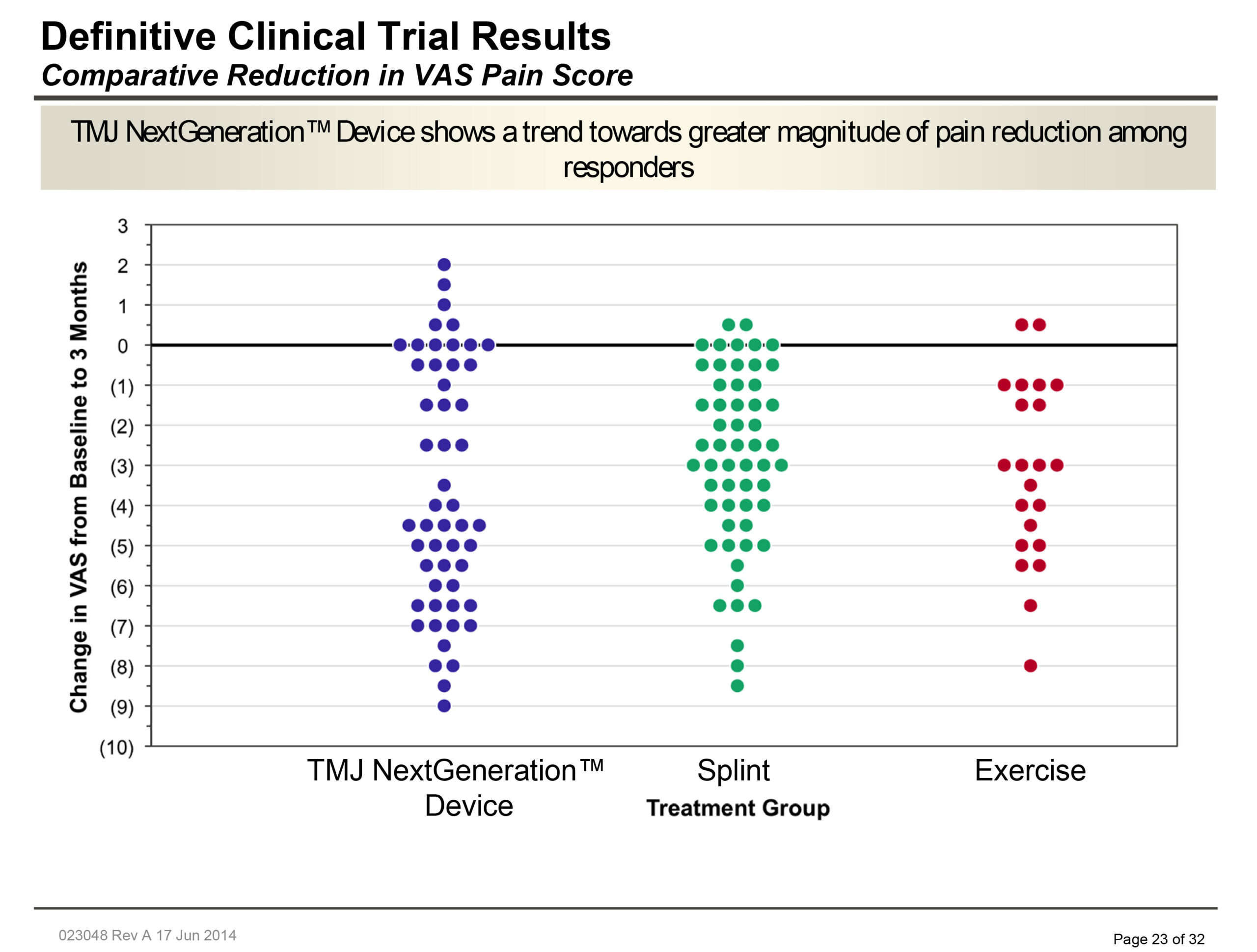
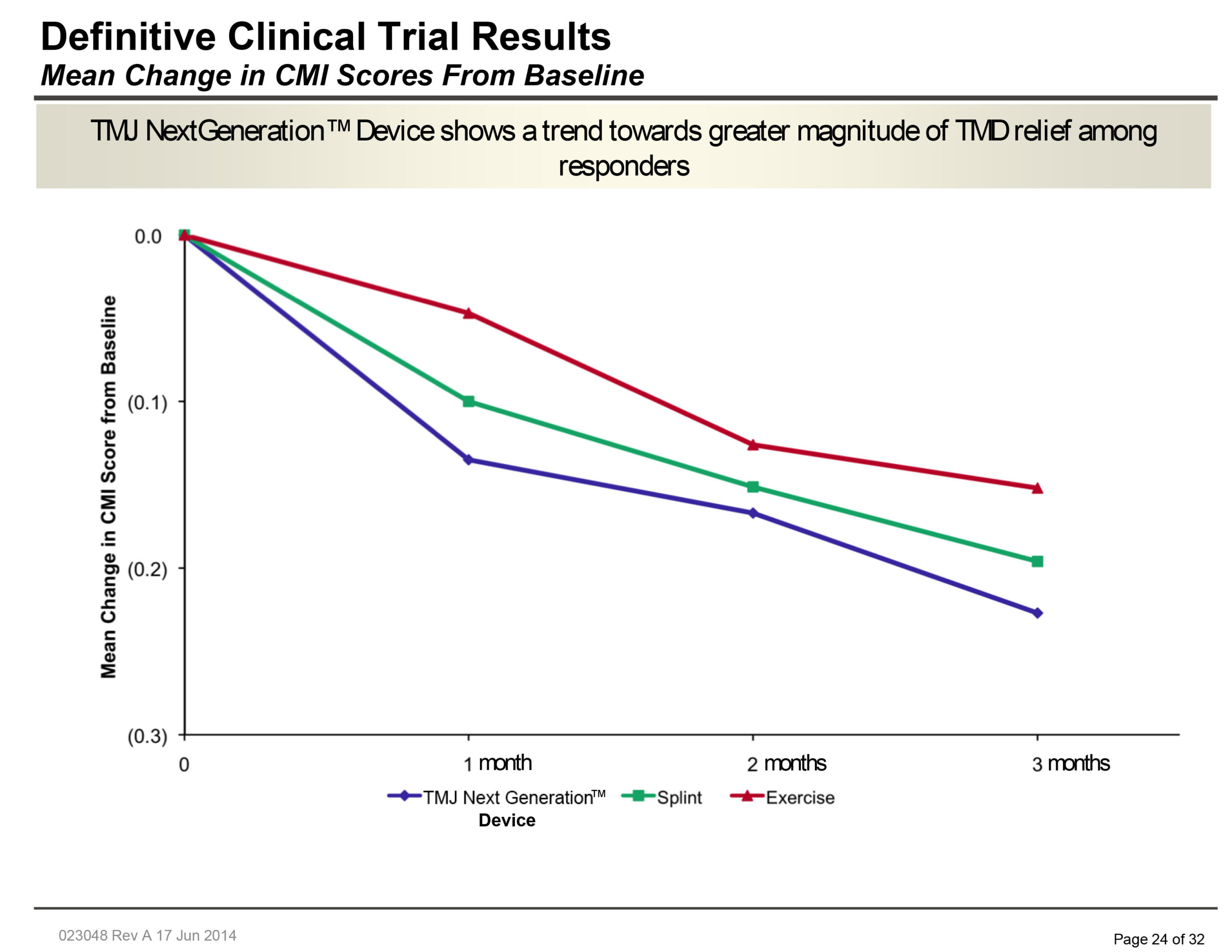
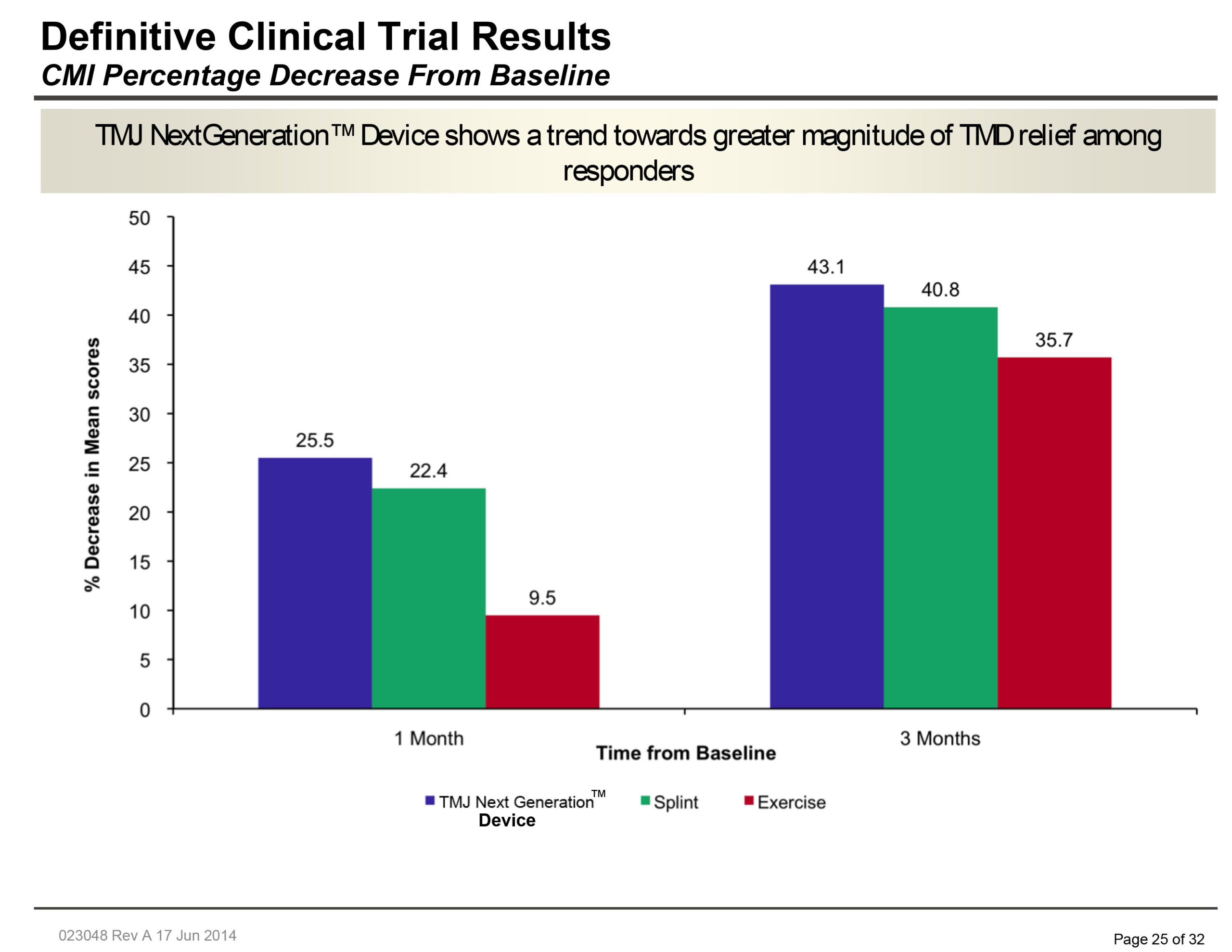
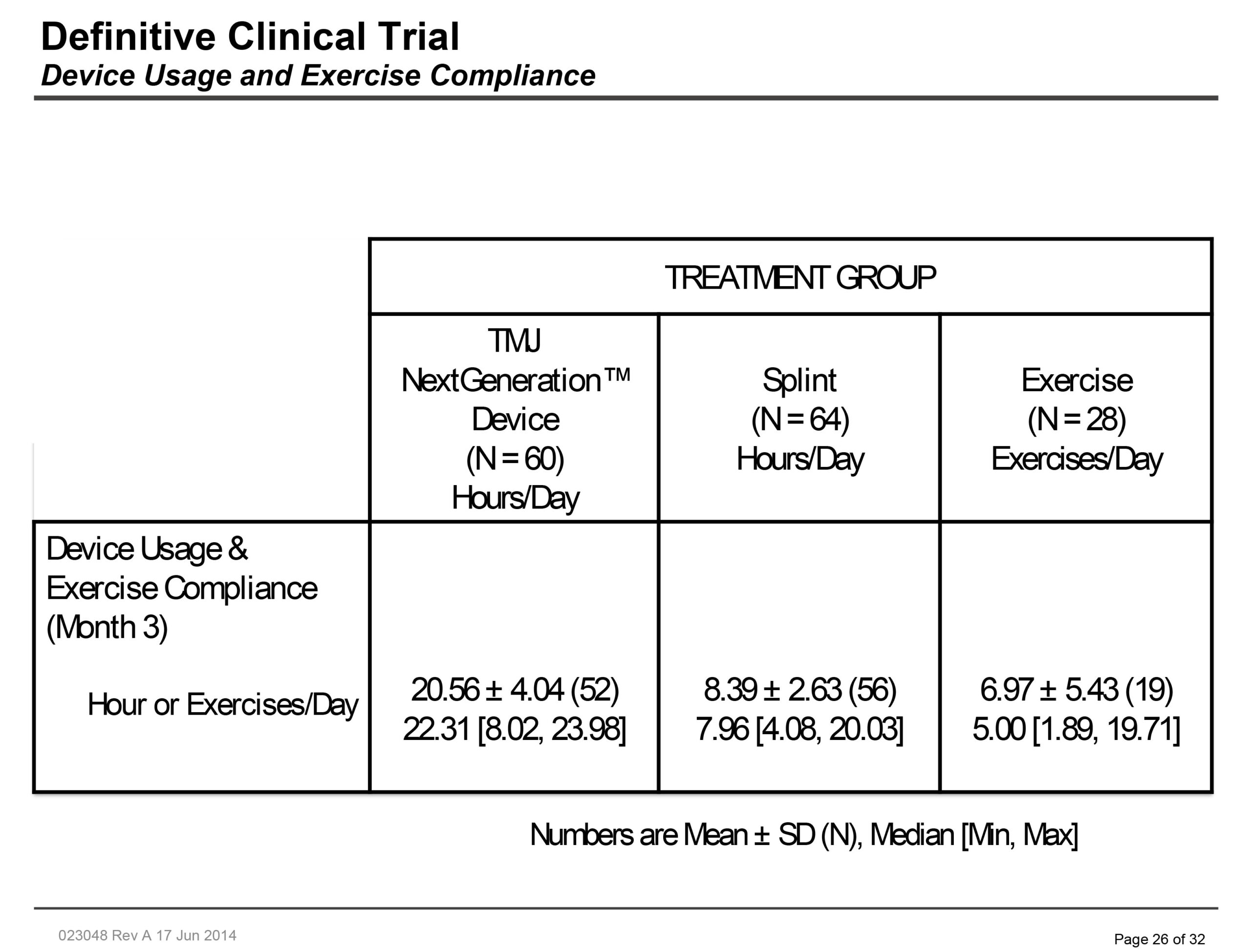
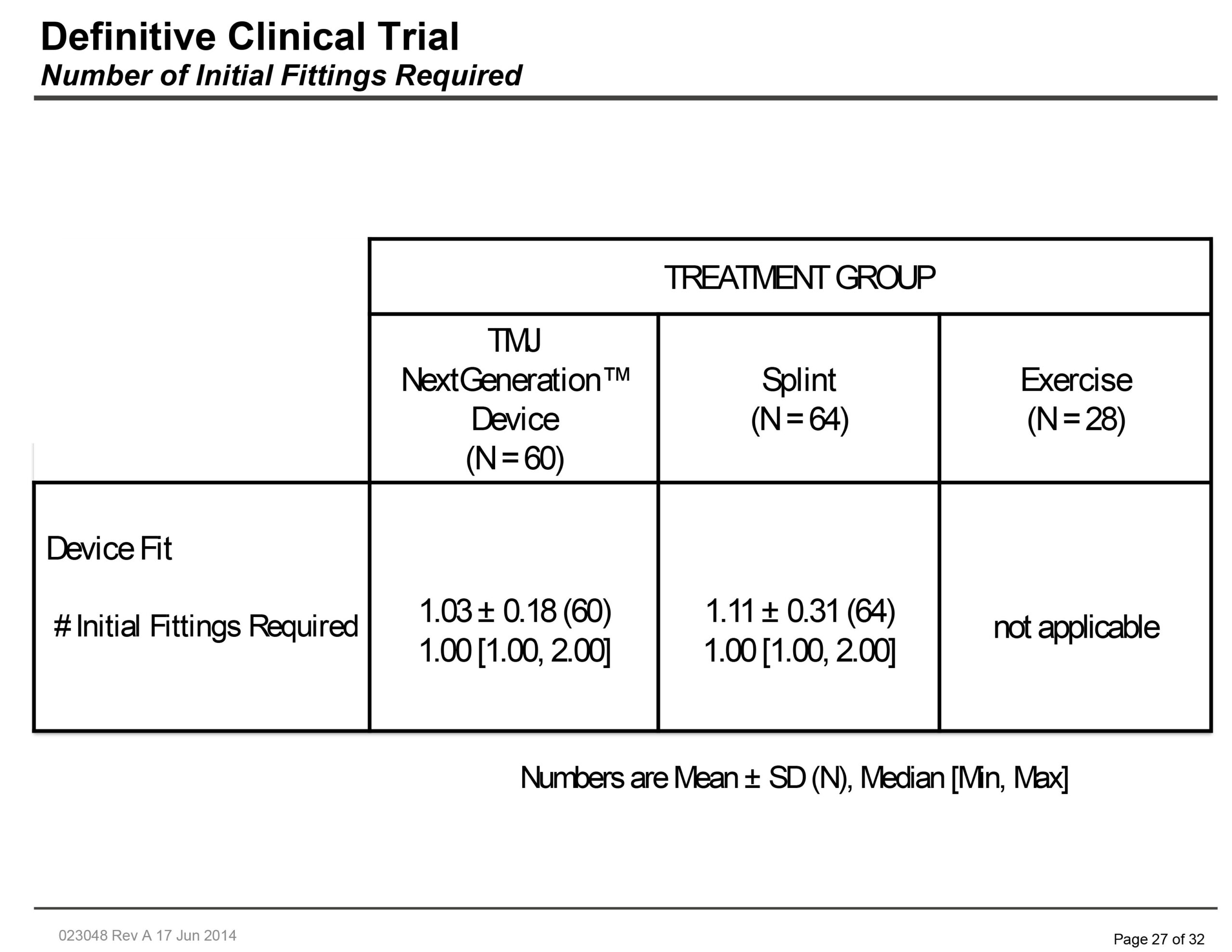
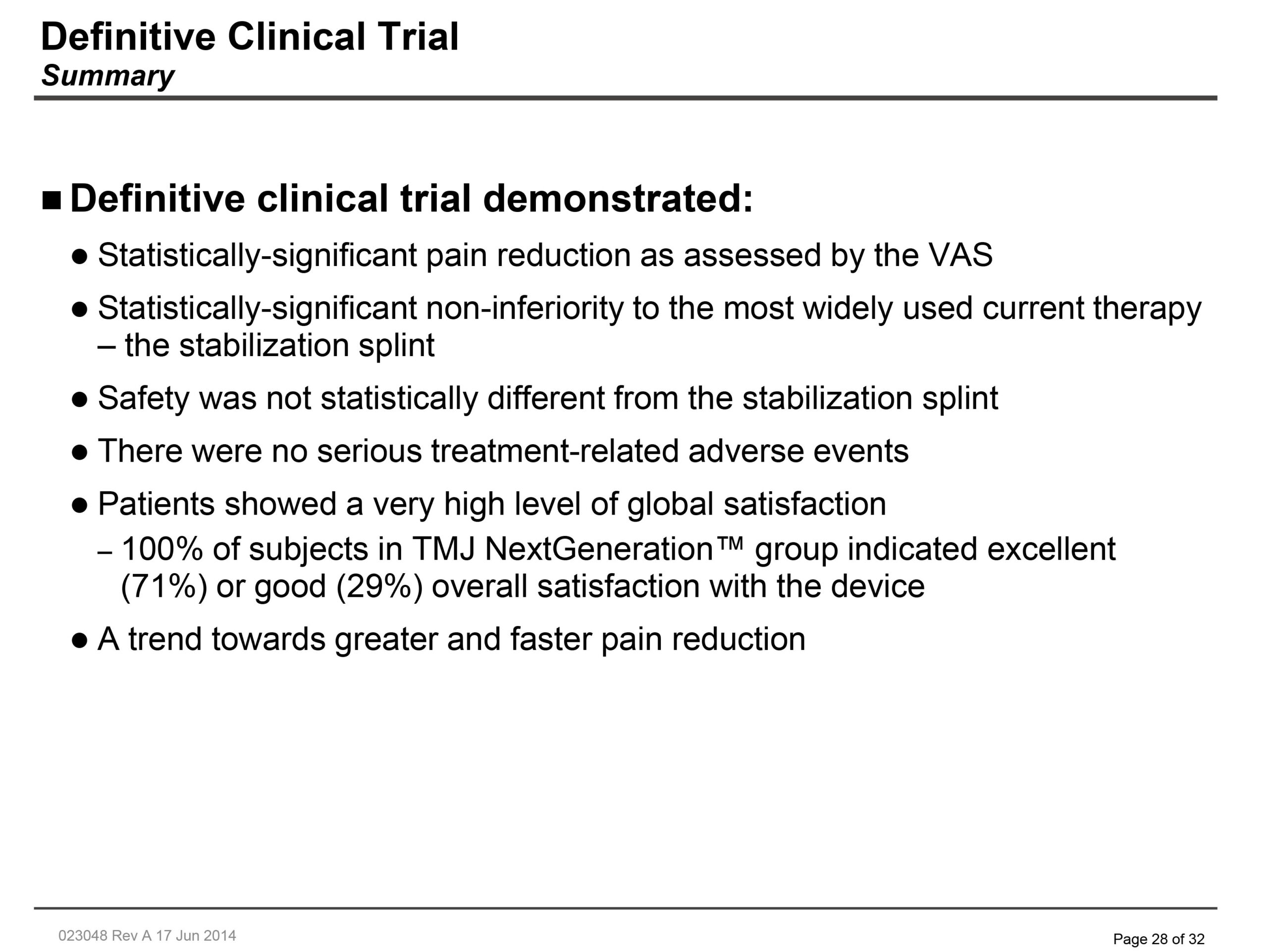
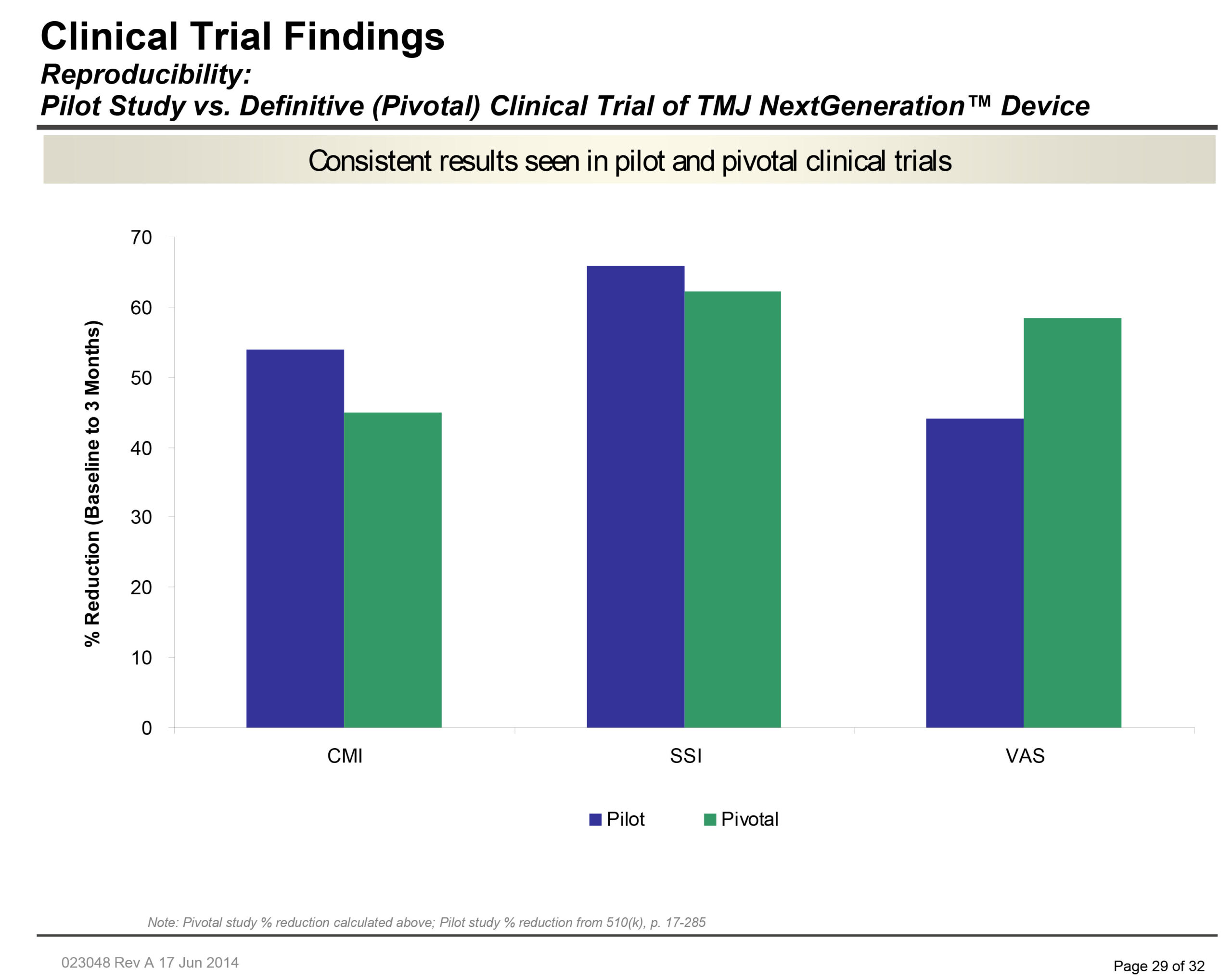
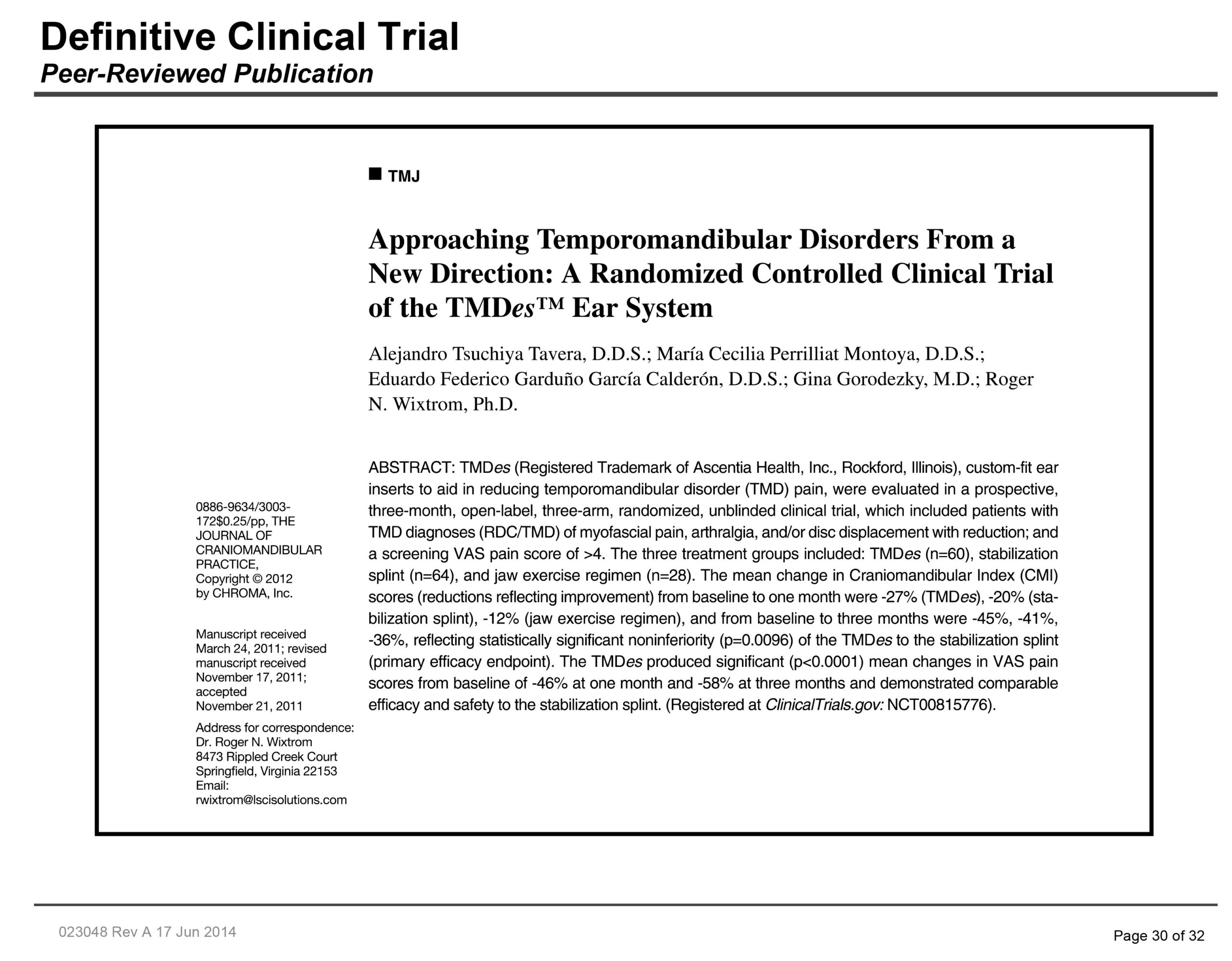
Treating TMJ comes with many different processes with varying degrees of success. One of the solutions offered at Dr. Goldberg’s ENTFPS offices includes the TMJ NextGeneration™ Device, a revolutionary new prosthetic tool that patients insert comfortably into their ear canals without any restrictions to their hearing. Through clinical trials run by Roger N. Wixtrom, Ph. D. et al., patients who received treatment from this ear insert saw significantly reduced pain faster than the more commonly used stabilization splints. These patients experienced no significant adverse effects or safety concerns from the TMJ NextGeneration™ Device. You can view full details regarding the clinical trial below:
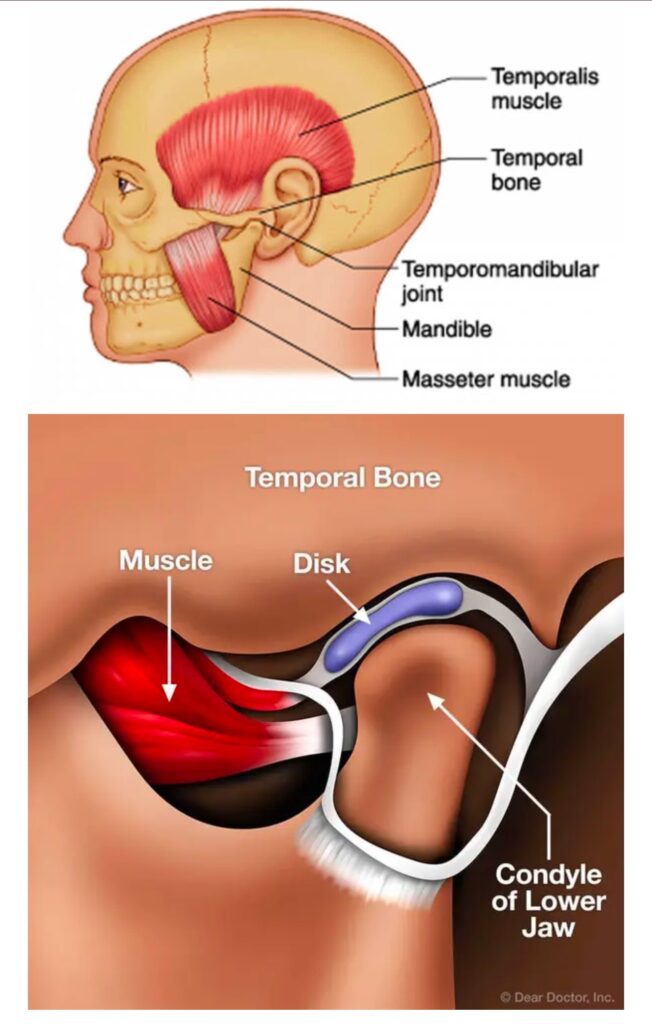
TMJ (temporomandibular joint) disorders can cause a variety of symptoms. These typically affect the jaw, face, and surrounding areas. Common symptoms include:
We recently sat down with a patient who was suffering from TMJ disorder. Dr. Friedman explained to the patient that this disorder was causing pain in his jaw and contributing to his frequent, inconsolable headaches. Then Dr. Goldberg outlined a number of treatment options, including one that came as a bit of a surprise.
“Have you considered Botox therapy for your TMJ?”
Our patient did a double-take, “Botox for TMJ? I’ve never heard of that before, how does that work?”
Here’s what he told him.
Most people know it as a beauty-enhancing product that gets rid of wrinkles and fine lines in the face. That’s true, it is! But think about what Botox does — it temporarily prevents nerve cell signals from reaching your muscles and reduces abnormal muscle contractions. With this in mind, you can understand how it can be useful for relaxing the muscles around your jaw, too.
In fact, Botox has a long history of medically therapeutic uses, all involving muscular conditions. Currently, Botox is used to treat over 20 different medical conditions, and there are more than 6 million Botox treatments administered each year.
Botox injections have been administered in dentists’ offices throughout the US for many years now. Some dentists do offer Botox as the finishing touch to a cosmetic dental treatment.
Here in our office, the use of Botox in dentistry stems from one important goal… relieving TMJ pain and helping you feel your very best.

The exact cause of BMS is not fully understood, which is why it’s often referred to as a “syndrome” rather than a disease. However, researchers have identified several potential contributing factors, which can be categorized into primary and secondary causes:
When no underlying medical or dental cause can be identified, the condition is classified as primary BMS. It is believed to be related to nerve dysfunction or damage in the oral cavity, possibly involving the nerves responsible for taste and pain.
Secondary BMS occurs when the burning sensation is linked to an underlying condition or factor, such as:

Living with BMS can be challenging, but there are steps you can take to cope with the condition:
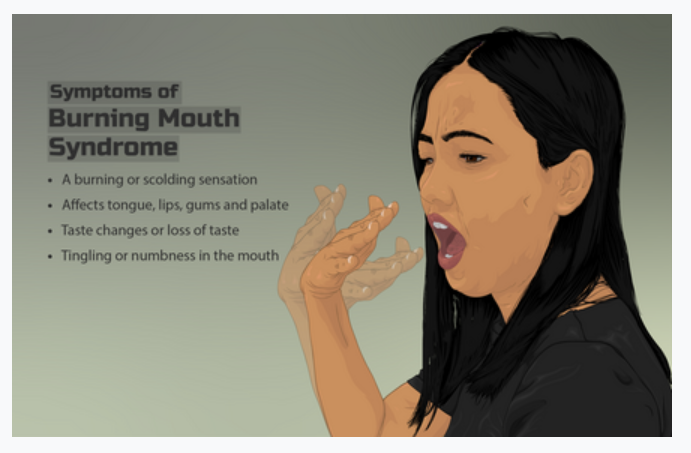
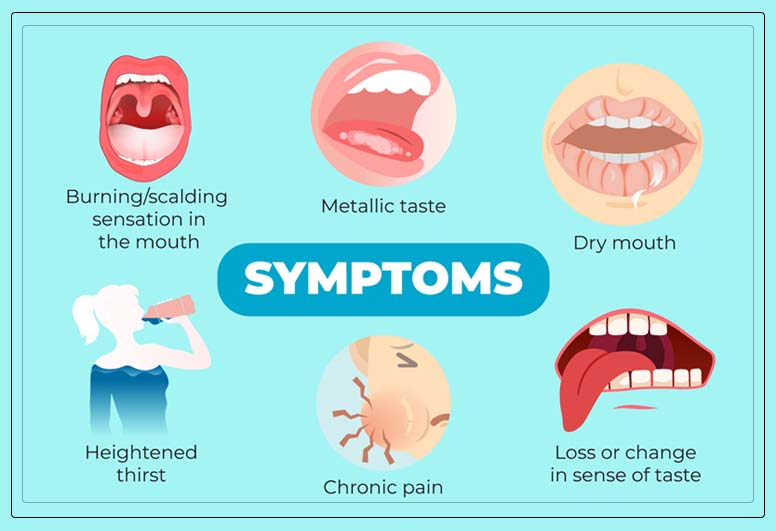
Burning Mouth Syndrome is a chronic condition characterized by a burning or scalding sensation in the mouth, often without any obvious cause. The discomfort can affect the tongue, lips, gums, palate, throat, or the entire mouth. For some, the sensation is mild and intermittent, while for others, it can be severe and persistent, significantly impacting their quality of life.
BMS is more common in middle-aged or older adults, particularly women going through menopause, though it can affect anyone. Despite its prevalence, diagnosing BMS can be challenging because it often overlaps with other oral health issues or systemic conditions.
The primary symptom of BMS is, of course, a burning sensation in the mouth. However, this condition can also present with other accompanying symptoms, such as:
The burning sensation may fluctuate throughout the day, often worsening as the day progresses. Some people report temporary relief while eating or drinking, which can make the condition even more perplexing.
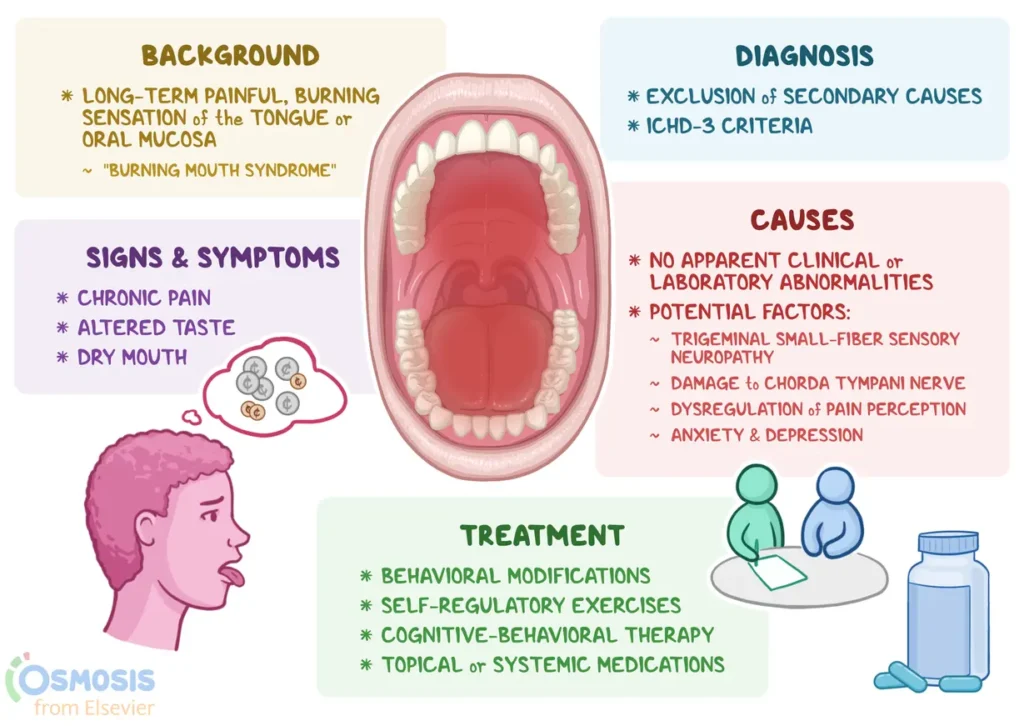
Diagnosing BMS can be a process of elimination. Your healthcare provider or dentist will likely start by reviewing your medical history, conducting a physical examination, and ruling out other potential causes of your symptoms. They may also order blood tests to check for nutritional deficiencies, hormonal imbalances, or other systemic issues.
In some cases, a referral to a specialist, such as an oral pathologist or neurologist, may be necessary to confirm the diagnosis.
While there is no one-size-fits-all cure for BMS, several treatment options can help manage the symptoms and improve your quality of life. The approach will depend on whether your BMS is primary or secondary:
If an underlying cause is identified, treating that condition often alleviates the burning sensation. For example:
When no specific cause is found, treatment focuses on symptom management. Options may include:
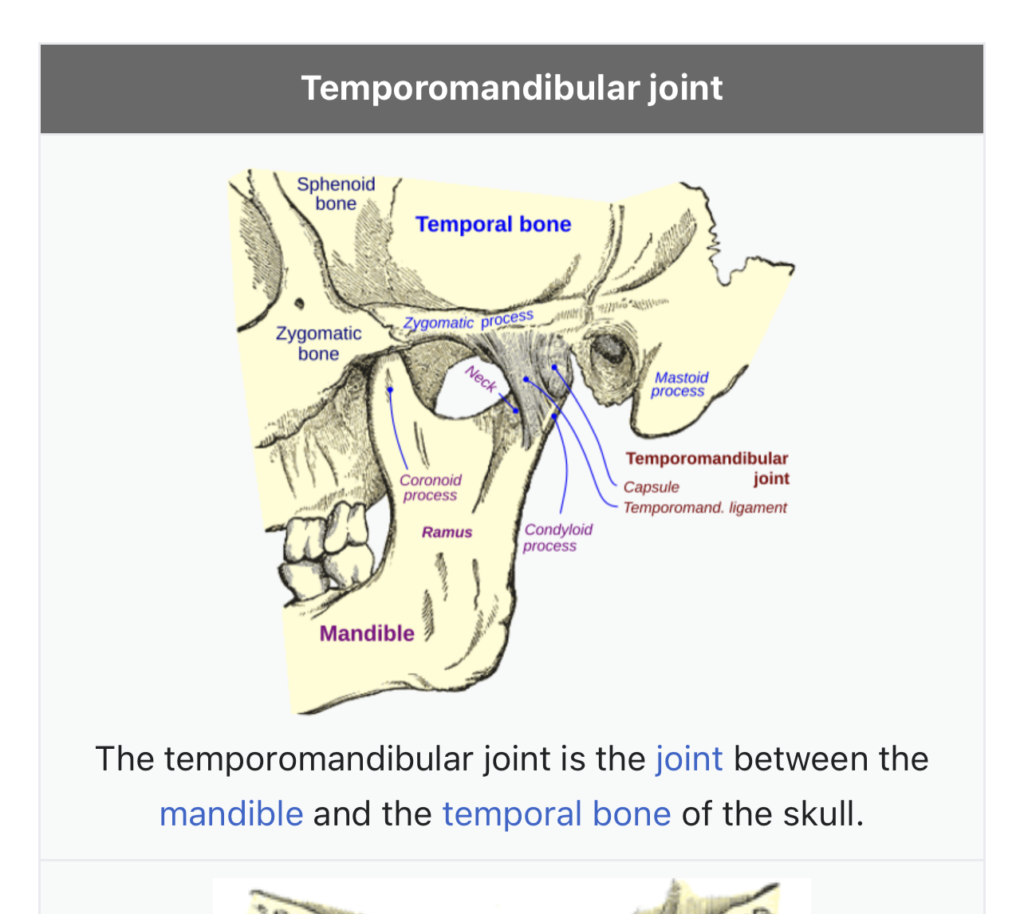
Temporomandibular Join (TMJ) arthritis is a common cause of orofacial pain with distressing symtomps.
The patients most commonly females are often anxious and worried due to typical gritty sound produced during chewing moments.
In other cases there is pain followed by decreased mouth opening.
Currently the treatment is not standardised though the clinicians are treating these disorders either by oral medications, splintage or by injections. Though local injection of Triamcinolone acetonide and Hyaluronic acid is an innovative therapy, yet it is elusive of much research.
Most injections of Botulinum Toxin A For TMJ will last approx. 3-4 months. Immediately following your treatment, you should be able to return to normal function. The instructions you may have given include:
The areas where the injections were given.
These 6 at-home treatments for TMJ disorders may help you.
Choose the right foods: Eating soft foods, such as mashed potatoes and applesauce, can decrease jaw pain and discomfort. If you do eat hard foods (eg, raw carrots), be sure to cut them into tiny pieces or take very small bites. Also, eating sticky or chewy foods—and even chewing gum—can aggravate your symptoms, so limit these types of food.
Do jaw exercises: Jaw stretches and other face exercises can help ease TMJ disorder symptoms. Your doctor, dentist, or a physical therapist can show you how to do at-home jaw exercises to stretch your jaw muscles. He or she can also show you how to massage the muscles in your jaw.
Learn stress management techniques and do them frequently: Stress can aggravate TMJ pain—and that’s why stress management techniques are so important to do. Examples of ways to control your stress at home are doing yoga poses, deep breathing, guided imagery, and meditation.
Limit extreme jaw movements: Yawning and yelling are examples of extreme jaw movements that can place tension on the TMJ. Be aware of overusing your jaw muscles because it can lead to jaw strain.
Use heat or cold therapy: Applying moist, warm heat packs or ice packs to your jaw can help to relax your jaw and face muscles. Your doctor will let you know how long to leave the ice pack or heat pack on, as well as the proper placement of the packs.
Wear a bite guard: You can wear a bite guard (also called a stabilization splint) to help keep you from grinding or clenching your teeth. Bite guards are usually made of plastic; they fit over your upper and lower teeth, and they prevent your teeth from touching. There are numerous types of bite guards available—you can wear a soft or firm bite guard, for example.
Bite guards should only be used temporarily (your doctor or dentist will let you know how long and how often to wear it). If the bite guard increases your pain or is beginning to change how you bite, stop using it immediately and call your doctor.
Adding these at-home treatments to your overall treatment plan for TMJ disorders can help make your TMJ disorder a lot easier to deal with. When doing these treatments, be sure to note your symptoms. If your TMJ symptoms get worse or you have new symptoms, talk to your doctor right away.
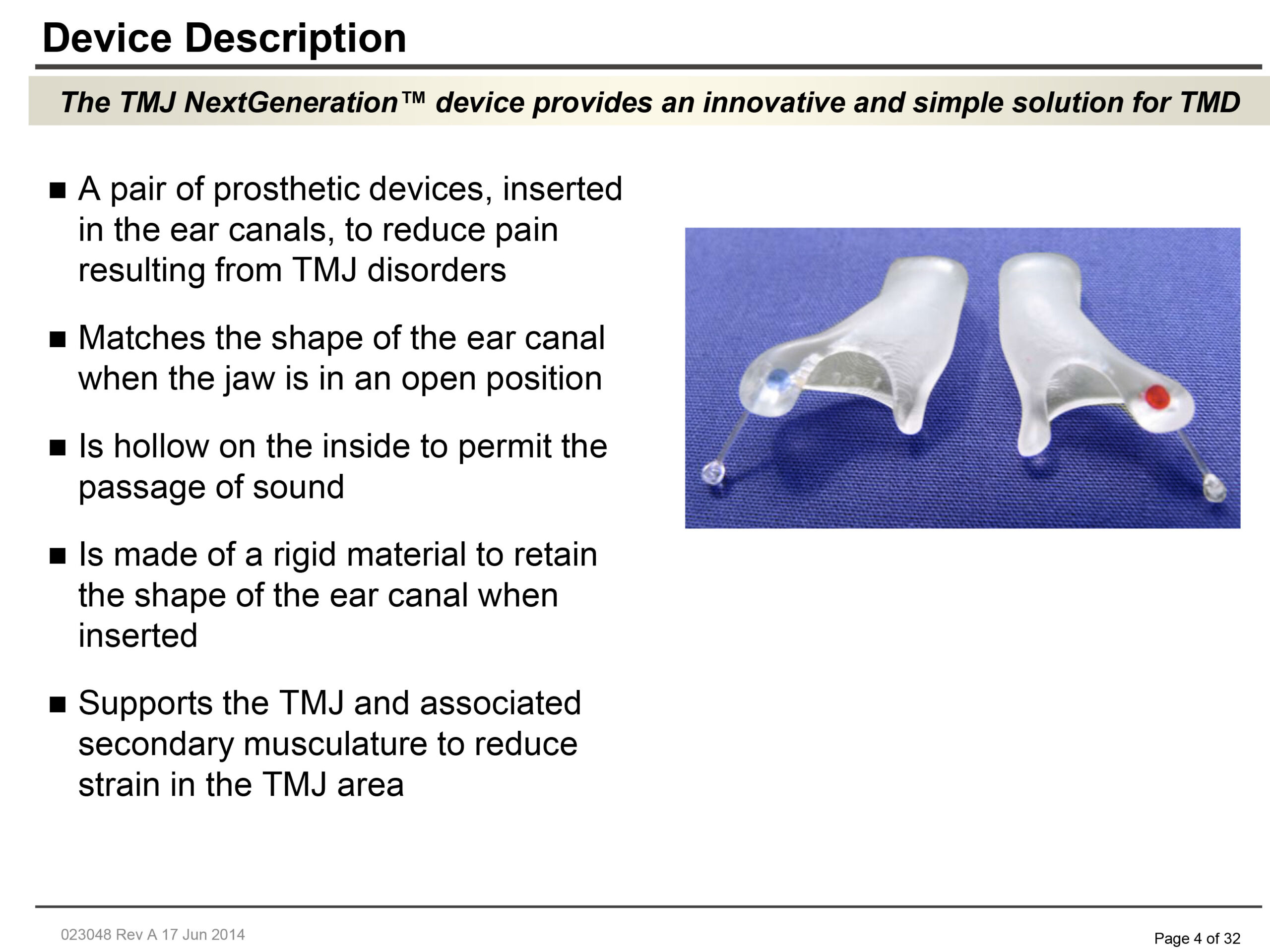
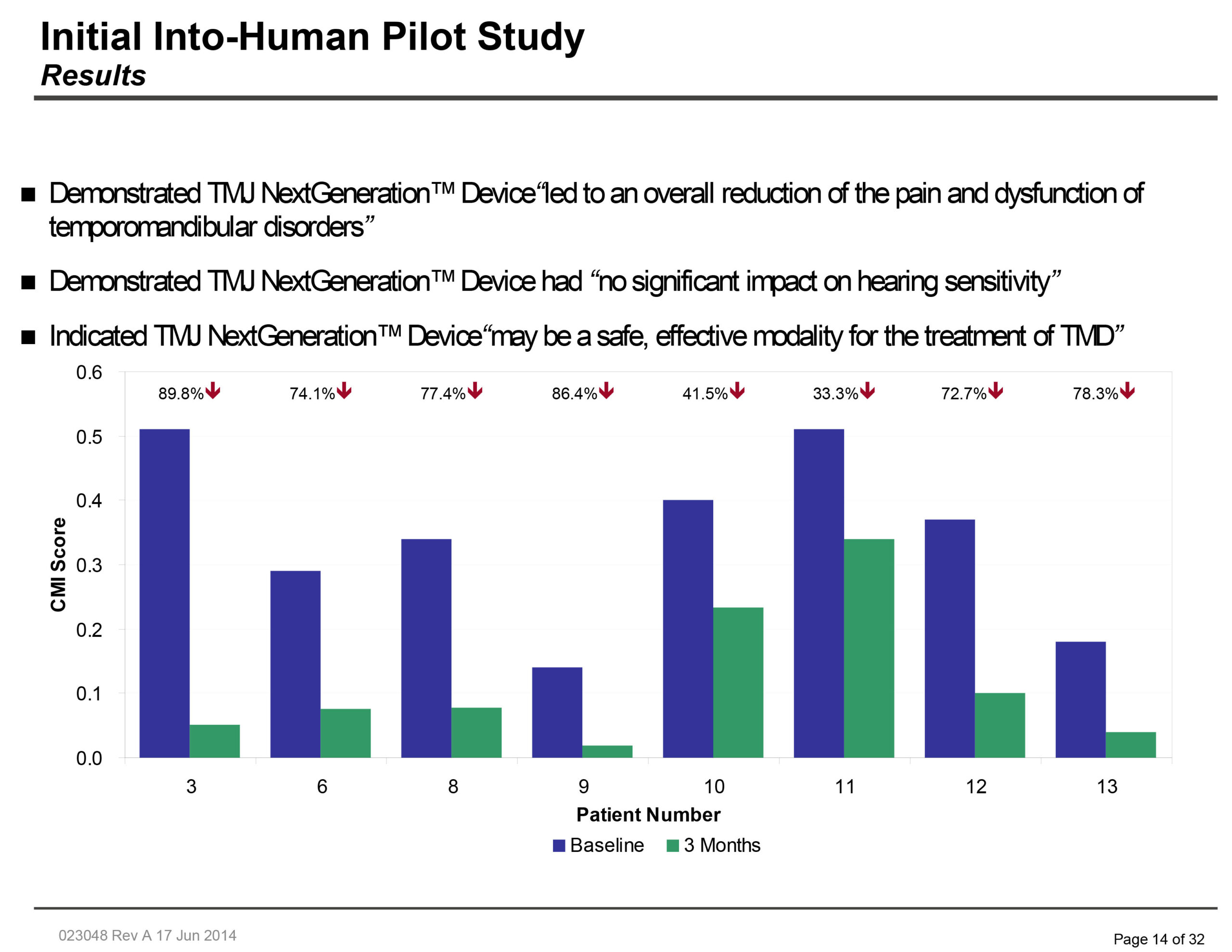
If you believe that the TMJ NextGeneration™ Device is right for you, contact Dr. Goldberg to schedule your next appointment!